Clinical Case Studies

The scaphoid bone is the largest bone of the proximal row of wrist bones and is the most fractured during a fall on outstretched hand injury (FOOSH). If diagnosed and treated early, 90% of acute scaphoid fractures heal with no complications. Delayed diagnosis and treatment can lead to complications including non-union, delayed union, and avascular necrosis. Current diagnostic modalities used to detect a scaphoid fracture include conventional radiograph, CT, magnetic resonance imaging (MRI), bone scintigraphy, and sonograms.
High resolution enables visualization and quantification of both cortical and trabecular density, as well as characterizing the morphology of the fracture site. Visualization of ligament injuries and cartilage degeneration is also possible. Improved imaging, particularly around the bone/metal interface, has the potential to significantly reduce the uncertainties associated with surgery, resulting in improved patient outcomes.
Since late 2019, MARS has been conducting human trials out of the University of Canterbury (see case studies below). We are excited to announce we are moving our human trials into two clinics, one in Christchurch, New Zealand and one in Europe. These scanners will be used to assess real patient situations and provide us with valuable data regarding clinician workflow, before they are introduced into clinics.
Case study one
A 56-year-old-woman, who is right hand dominant, fell onto her outstretched hand hyperextending her wrist. The patient has x-ray radiographs, CT scans, and a cone beam CT (CBCT) scan to assess fracture healing due to ongoing pain and tenderness of her left wrist. The MARS scan was performed seven months post injury.
Results: The MARS images show a comminuted transverse fracture at the scaphoid waist. Sclerosis was observed at the fracture margin seven months post injury indicating non-union. Sagittal images show collapse at the fracture site with humpback deformity. Proximal pole sclerosis was not observed.
Clinical relevance: The MARS scanner produces high contrast bone detail, as well as assessment of bone density and morphology at the fracture site. This increased level of detail and information can aid in treatment decisions, as well as surgical planning.
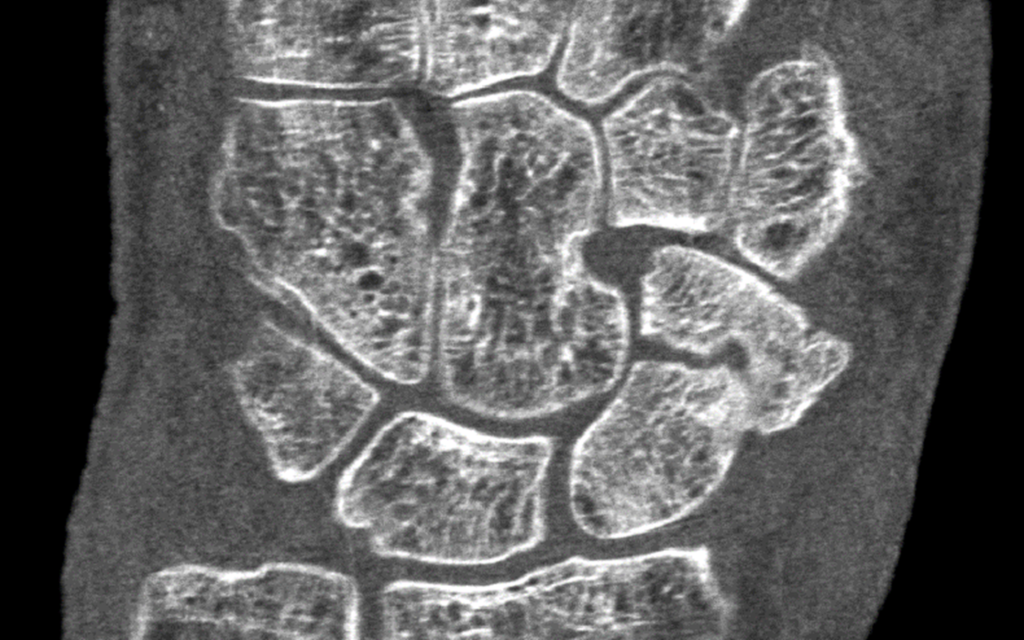
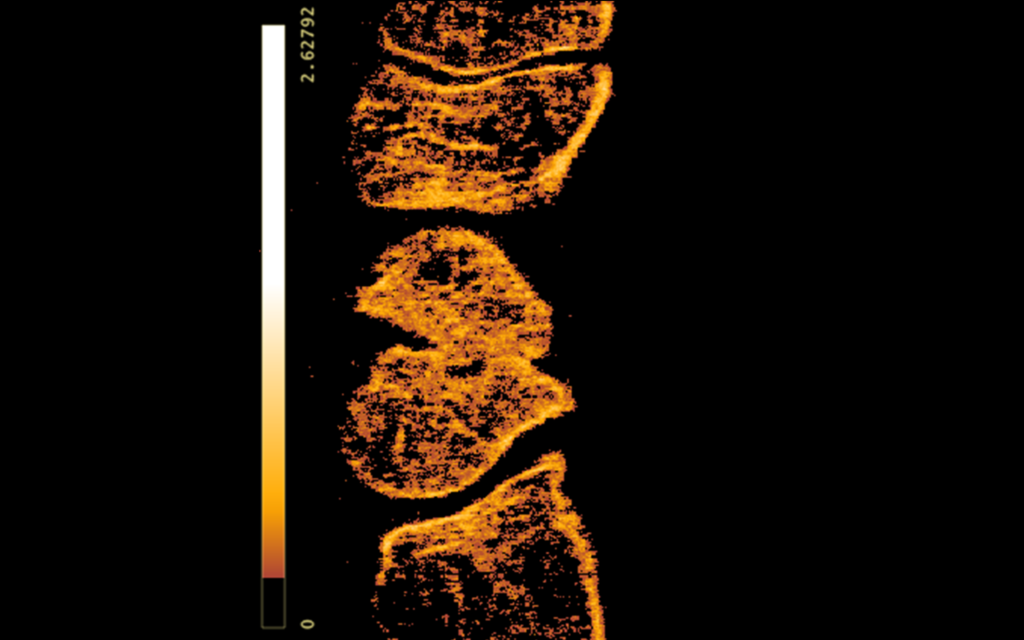
Figure Left: Coronal view of the left wrist showing comminuted transverse fracture at the scaphoid waist. Right: Sagittal calcium imaging demonstrates sclerosis of the scaphoid fracture site and humpback deformity. The color code represents the density of the calcium channel.

3D volume rendering of the patient’s wrist differentiating soft tissue and bone.
Case study two
A 55-year-old right hand dominant male was troubled with chronic right wrist pain following a bike crash. The patient had radiographs and CBCT scan to monitor the progress of fracture healing. Twelve weeks post injury, the patient had a MARS scan.
Results: The MARS images show non-union with displacement. Small bony fragments were observed at the fracture margin. The separation between the fracture fragments was more than 3 mm. Sclerosis was not observed.
Clinical Relevance: The MARS scanner produces high contrast bone detail, as well as assessment of bone density and morphology at the fracture site. This increased level of detail and information can aid in treatment decisions, as well as surgical planning.
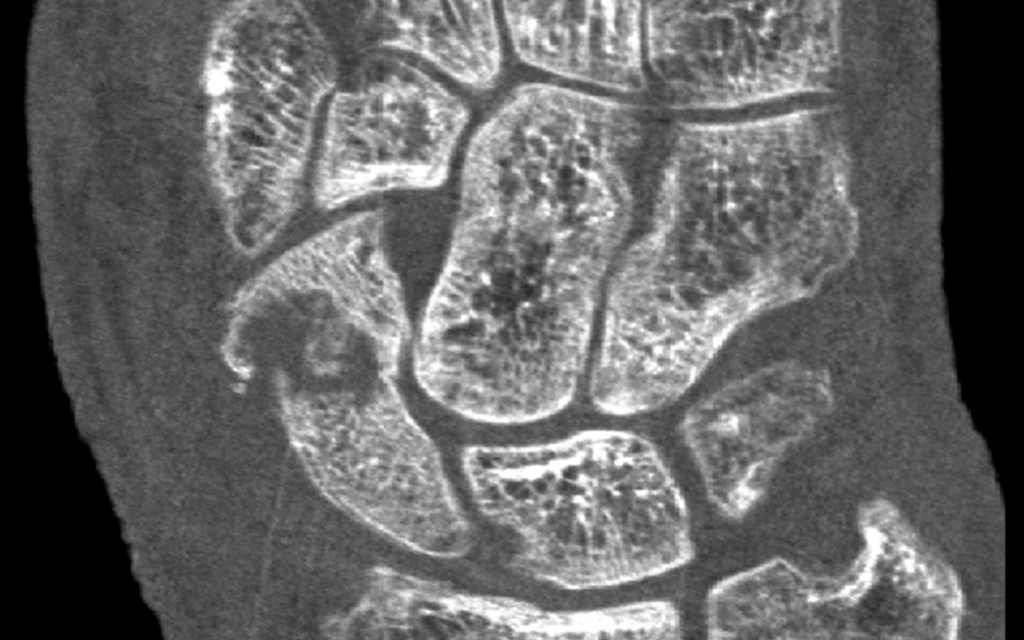

Figure Left: Coronal view of the right wrist demonstrates the separation between the fracture fragments. Right: Sclerosis of the fracture margins was not observed on calcium material imaging (right).
Case study three
A 22-year-old man fell from his bike onto an outstretched hand injuring his left wrist. The patient had an open reduction and internal fixation. Two months post operation, the patient had a MARS scan.
Results: MARS images show reduced metal artifacts at the bone-metal interface and visualisation of soft tissue in the vicinity of the implant. The MARS images show the impingement of the screw on the scaphotrapeziotrapezoidal (STT) joint. Sclerosis was observed at the proximal pole of the scaphoid suggesting avascular necrosis.
Clinical Relevance: Postoperative imaging evaluation of fracture fixation with metalware is often impaired by the metal artifact, which makes it difficult to evaluate the surrounding tissue. Due to reduced metal artifact and greatly improved visualisation of the bone-metal interface, MARS can be used to assess fracture healing and identify any metalware complications, such as implant loosening, migration of screw, or infection.
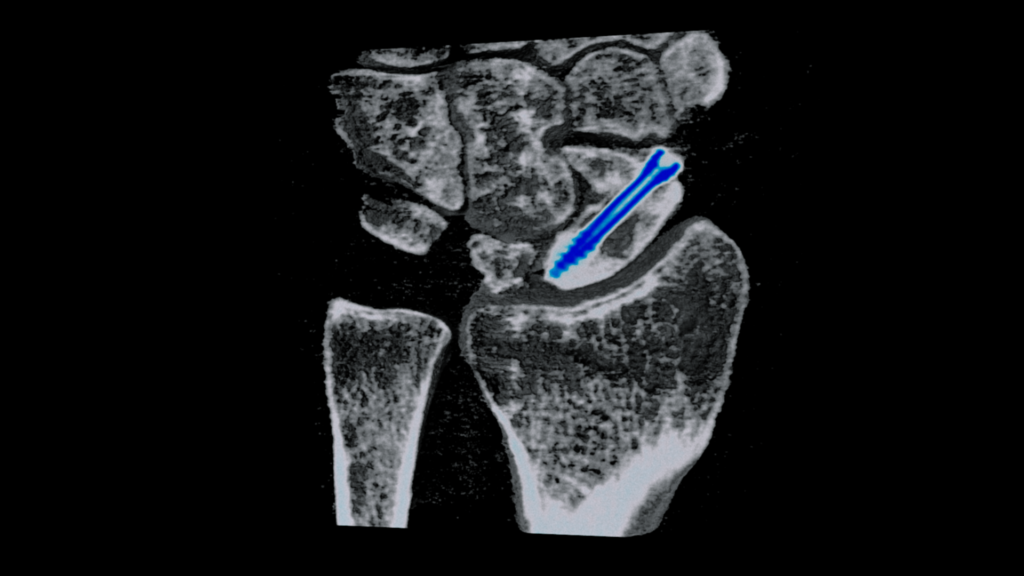
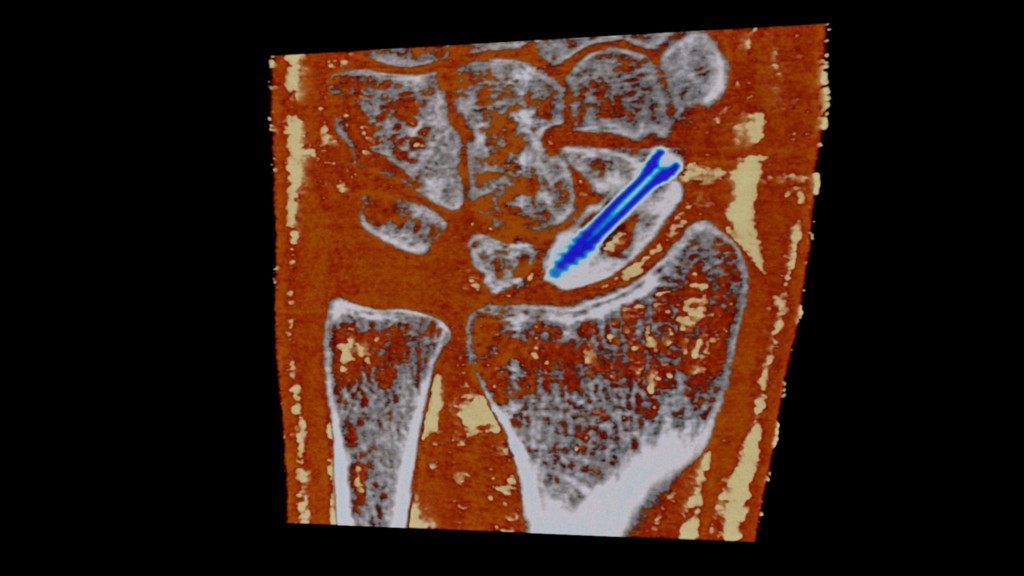
Figure: Coronal views of the left wrist show bone and soft tissue in the vicinity of the implant with reduced metal artifacts. The material image (right) demonstrates differentiation of tissues, fat (yellow), soft tissue (orange red), bone (grey), and screw (blue) (right).
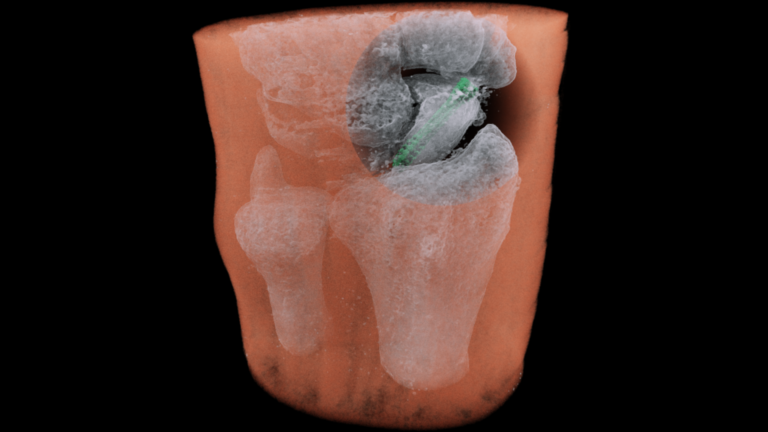
3D volume rendering of the patient’s wrist differentiating soft tissue, bone, and metallic screw.